Every person matters
A 60-year-old man presented to the hospital with chest pain shortly after returning from a ski trip, initially referred with a presumed diagnosis of pneumonia. His chest X-ray was unremarkable, troponin was negative, and there were no classic signs of infection, prompting further evaluation.
A bedside AISAP exam revealed a dilated IVC and moderately enlarged right ventricle, raising concern for right heart strain. Based on these findings, the care team pursued CT imaging, which confirmed pulmonary embolism (PE), leading to a timely and accurate diagnosis that may have otherwise been delayed.

A 89-year-old man with congestive heart failure and a TAVI performed four months earlier presented with shortness of breath and desaturation. A bedside AISAP exam revealed EF 18%, severe MR, severe TR, and an enlarged right atrium.A formal echocardiogram confirmed these findings, and he was referred for MitraClip as part of his comprehensive management plan.

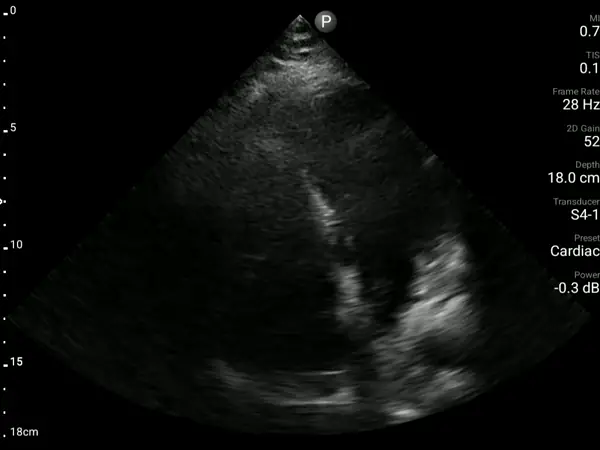
A 75-year-old woman with metastatic breast cancer arrived at the ED with worsening weakness and shortness of breath. AISAP revealed a large pericardial effusion, leading to the diagnosis of cardiac tamponade. She underwent urgent pericardial drainage, with 650 mL removed, resulting in rapid stabilization.
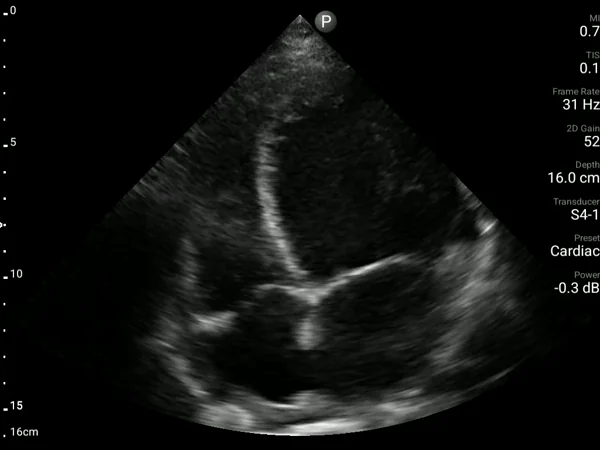
A 39-year-old woman with APLA syndrome returned to the ED three weeks after an emergency C-section with recurrent chest pain. Pulmonary embolism had been ruled out during a visit two days earlier, and an echocardiogram performed two months prior was normal (EF 60%).
A bedside AISAP exam revealed severe LV dysfunction, moderate RV dysfunction, severe MR, and mild pericardial effusion. These findings led to an urgent formal echocardiography and cardiology review, which established the diagnosis of postpartum cardiomyopathy.
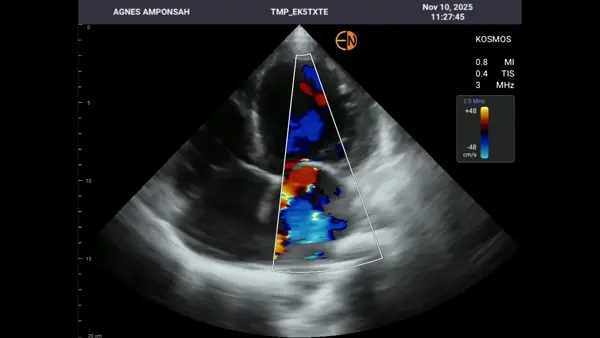
A 47-year-old woman with obesity, hypertension, dyslipidemia, and a history of chronic heart failure presented with shortness of breath, peripheral edema, and clinical signs of deterioration. Without on-site echocardiography, her worsening status could not be objectively assessed. A bedside AISAP exam revealed EF 14%, severe mitral regurgitation, and severe tricuspid regurgitation, confirming significant decline from her prior evaluation. In this low-resource setting, AISAP provided the essential diagnostic clarity needed to guide timely management during an acute heart failure exacerbation.
.webp)
A 46-year-old woman was admitted with palpitations, dizziness, and persistent tachycardia. Management for suspected ACS did not improve her condition for several days. A bedside AISAP exam revealed reduced RV Fractional Area Change and a dilated right atrium, findings that raised concern for pulmonary embolism.
With no on-site CT and expected delays for external imaging, AISAP provided supportive information that guided a change to therapeutic anticoagulation. The patient showed clinical improvement, and a subsequent CT scan confirmed the presence of PE.

A 95-year-old woman with no prior cardiac history arrived at the ED with shortness of breath. A bedside exam using AISAP identified severe aortic stenosis and left ventricular dysfunction, providing immediate diagnostic clarity and guiding referral for further evaluation that led to TAVI approval for the patient.

A 47-year-old man with a history of ischemic heart disease presented to the ED with chest pain. A bedside exam using AISAP identified severe heart failure with an ejection fraction of 27% within minutes, enabling swift referral to cardiology and timely, targeted treatment.

A 70-year-old man, healthy and recently after mitral valve replacement, arrived at the ED with new leg edema and shortness of breath. A bedside exam using AISAP revealed new heart failure within minutes, giving the care team immediate clarity and enabling rapid, targeted treatment.
































.png)